Interpretation of Abnormal Vital Signs and Appropriate Interventions
Interpreting abnormal vital signs in pediatric patients is crucial for assessing their health status, detecting underlying conditions, and determining the need for interventions. Abnormal vital signs can indicate a wide range of issues, from mild to life-threatening. The appropriate intervention depends on the specific abnormal vital sign and its context.
Here’s an overview of how abnormal pediatric vital signs might be interpreted, and the potential interventions that can be implemented:
1. Heart Rate (HR)-
Abnormal Findings:
-
Tachycardia: Heart rate > 160 bpm (newborns), > 130 bpm (children)
Potential Causes: Fever, dehydration, anemia, infection, hypoxia, pain, or anxiety.
Interventions: Correct the underlying cause (e.g., administer fluids for dehydration, antipyretics for fever, oxygen if hypoxic). Monitoring and frequent reassessment are important.
-
Bradycardia: Heart rate < 90 bpm (newborns), < 60 bpm (older children)
Potential Causes: Hypoxia, increased intracranial pressure, heart block, or vagal stimulation.
Interventions: Assess oxygenation (administer oxygen if necessary), ensure airway patency, consider cardiac monitoring. For persistent bradycardia, atropine or pacing may be required.
-
2. Respiratory Rate (RR)-
Abnormal Findings:
-
Tachypnea: Respiratory rate > 60 breaths/min (newborns) or > 40 breaths/min (older children)
Potential Causes: Fever, respiratory infections (e.g., pneumonia, bronchiolitis), asthma, hypoxia, pain, or metabolic acidosis.
Interventions: Administer oxygen if hypoxic, treat the underlying cause (e.g., antibiotics for infection, bronchodilators for asthma), and consider fluid management.
-
Bradypnea: Respiratory rate < 30 breaths/min (newborns) or < 12 breaths/min (older children)
Potential Causes: Central nervous system depression, opioid overdose, head injury, or severe hypoxia.
Interventions: Immediate assessment of airway and oxygenation, provide oxygen, reverse any narcotic overdose with naloxone if appropriate, and consider further medical evaluation for neurological issues.
-
3. Blood Pressure (BP)-
Abnormal Findings:
-
Hypertension: BP > 95th percentile for age and gender.
Potential Causes: Renal disease, heart disease, obesity, endocrine disorders (e.g., hyperthyroidism), or anxiety.
Interventions: Identify and treat underlying cause (e.g., antihypertensive medications, lifestyle modifications, or treatment for the specific condition causing hypertension). Frequent monitoring of BP is essential.
-
Hypotension: BP < 5th percentile for age or a drop of 20 mmHg below baseline.
Potential Causes: Dehydration, shock (hypovolemic, septic, or cardiogenic), bleeding, or adrenal insufficiency.
Interventions: Fluid resuscitation (IV fluids), administration of vasopressors or inotropes in shock, and immediate evaluation for the cause of hypotension.
-
4. Temperature (T)-
Normal Range:
97.9°F to 99.5°F (36°C / 36.5°C to 37.5°C)
-
Abnormal Findings:
-
Fever: Temperature > 100.4°F (38°C)
Potential Causes: Infection (bacterial, viral, etc.), dehydration, inflammatory conditions.
Interventions: Administer antipyretics (e.g., acetaminophen, ibuprofen), increase fluid intake, and monitor closely for signs of serious infection (e.g., meningitis, sepsis). In high fevers (>104°F), consider cooling measures, sponging, or cooling blankets.
-
Hypothermia: Temperature < 95°F (35°C)
Potential Causes: Cold exposure, sepsis, metabolic disorders, or drug overdose.
Interventions: Warm the child gradually (e.g., using warm blankets, heated fluids), monitor for rewarming shock, and assess for other underlying causes (e.g., infection, drug toxicity).
-
Preventative Approaches
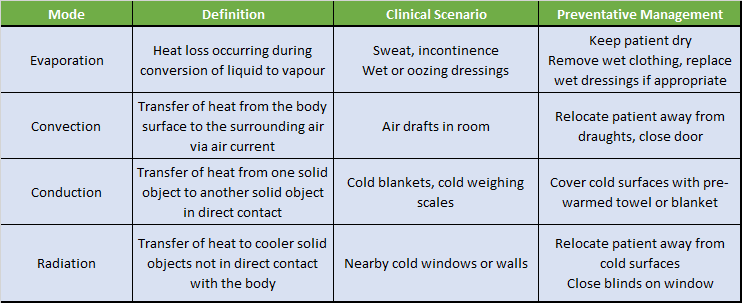
A patient’s surrounding environment can greatly impact their ability to maintain an otherwise stable body temperature. Acknowledging and minimizing environmental influences on thermoregulation is important for all pediatric patients, especially the neonatal and at-risk patient populations.
The table below outlines approaches nurses, clinicians and families can utilize towards minimizing preventable heat transfer from patients to their surroundings.
5. Oxygen Saturation (SpO2)-
Normal Range:
95% (for healthy children)
-
Abnormal Findings:
-
Hypoxemia: SpO2 < 90-92%
Potential Causes: Respiratory or cardiac issues (e.g., asthma, pneumonia, congenital heart defects, or respiratory distress syndrome).
Interventions: Administer oxygen, monitor closely, and treat the underlying cause (e.g., antibiotics for pneumonia, bronchodilators for asthma). Continuous monitoring is essential for critical patients.
-
Hyperoxia: SpO2 > 100%
Potential Causes: Overuse of supplemental oxygen.
Interventions: Adjust oxygen flow rates and monitor for oxygen toxicity, especially in neonates or patients with certain lung conditions (e.g., prematurity).
-
6. Capillary Refill Time (CRT)Normal Range: < 2 seconds
-
Abnormal Findings:
-
Prolonged CRT: > 2 seconds
Potential Causes: Poor circulation, shock, dehydration, or hypoxia.
Interventions: Evaluate for signs of dehydration or shock, administer fluids, and monitor perfusion. If associated with respiratory or cardiac distress, address oxygenation and circulation immediately.
-