Case Studies and Practice Scenarios
Sample Case using Modified Aldrete Scoring
Practice Scenario: 9-Month-Old After Inguinal Hernia RepairBackground:
A 9-month-old infant undergoes a laparoscopic inguinal hernia repair. The procedure takes 45 minutes, and general anesthesia is administered using a combination of inhalational agents. The infant has no significant comorbidities, but a family history of anesthesia sensitivity is noted. Postoperatively, the child is transferred to the PACU for observation.
Assessment in PACU:
-
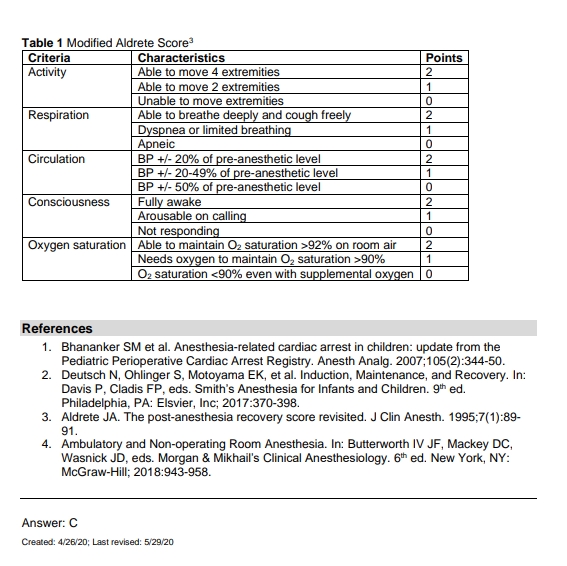
Activity (Mobility):
The infant is awake, moves arms and legs spontaneously, but is not able to follow commands.
Score: 1 (The infant moves two extremities voluntarily but cannot follow commands.)
-
Respiration (Respiratory Function):
The infant’s respiratory rate is 35 breaths per minute, and oxygen saturation is 97% on room air. The infant is not exhibiting signs of respiratory distress.
Score: 2 (Normal respiratory rate and oxygen saturation.)
-
Circulation (Blood Pressure):
The infant’s blood pressure is 80/55 mmHg, which is within expected range for age.
Score: 2 (Blood pressure is within 10% of baseline.)
-
Consciousness (Level of Consciousness):
The infant is drowsy but responds to tactile stimuli by moving and opening eyes. The infant does not yet respond to verbal stimuli.
Score: 1 (The infant is drowsy but responsive to touch.)
-
Oxygen Saturation (Peripheral Oxygenation):
Oxygen saturation is 97% on room air.
Score: 2 (Oxygen saturation is above 92% on room air.)
Total Aldrete Score:
Activity (1) + Respiration (2) + Circulation (2) + Consciousness (1) + Oxygen Saturation (2) = 8
Interpretation:
The infant has a total score of 8, indicating that the child is not yet fully ready for discharge from the PACU. The child needs more time to recover and should be monitored until the consciousness and activity scores improve. Specifically, the child should become more alert and demonstrate full movement of all extremities before being cleared for discharge.
Case Study 2: 6-Year-Old After AppendectomyBackground:
A 6-year-old child undergoes an appendectomy due to acute appendicitis. The surgery lasts about 1 hour, and the child is administered general anesthesia, which includes inhalational agents and muscle relaxants. The child has no significant medical history and no complications during the procedure.
Assessment in PACU:
-
Activity (Mobility):
The child is awake, slightly groggy, but able to move all four limbs. She is able to lift her legs and arms, although she seems slightly weak.
Score: 2 (The child can move all four extremities voluntarily.)
-
Respiration (Respiratory Function):
The child’s respiratory rate is normal (18 breaths per minute), with no signs of distress. Oxygen saturation is 100% on room air.
Score: 2 (Normal respiratory rate and oxygen saturation.)
-
Circulation (Blood Pressure):
The child’s blood pressure is 105/70 mmHg, which is normal for her age.
Score: 2 (Blood pressure is within 10% of baseline.)
-
Consciousness (Level of Consciousness):
The child is awake, alert, and responding appropriately to verbal commands. She is aware of her surroundings and able to speak clearly.
Score: 2 (The child is fully awake and alert.)
-
Oxygen Saturation (Peripheral Oxygenation):
The child’s oxygen saturation is 100% on room air.
Score: 2 (Oxygen saturation is above 92% on room air.)
Total Aldrete Score:
Activity (2) + Respiration (2) + Circulation (2) + Consciousness (2) + Oxygen Saturation (2) = 10
Interpretation:
With a total score of 10, the child meets all criteria for recovery and is ready for discharge from the PACU. The child is fully alert, breathing normally, and has stable cardiovascular parameters. After further assessment for pain management and confirmation that the child is comfortable, she can be safely transferred to a hospital room or discharged home, depending on the postoperative plan.