Criteria for Safe Discharge from PACU
Patients spend the immediate postoperative period in a post anesthesia care unit (PACU) so that they can be monitored for life-threatening complications, clearance of general or regional anesthetic medications and reversal agents and return to their previous level of functioning (or as close to it as possible given the surgical procedure). Airway maintenance, hypoxemia, and hypoventilation are primary concerns during the early post anesthesia phase, followed closely by hemodynamic stability. Promoting comfort by managing the patient's pain, nausea, and vomiting and maintaining normothermia are also essential aspects of care in the PACU.
Post anesthesia care is separated into phase I, phase II, and extended observation. Phase I is the initial recovery phase, during which the patient's stability is determined. The patient is most prone to complications during this phase. After meeting certain criteria, outpatients progress to phase II for treatment of any lingering complications, such as nausea, vomiting, and sleepiness. The patient and family should receive instructions for ongoing care at home and for follow-up care with the surgeon.
After the patient has recovered from anesthesia and has no significant complications, the patient is typically transferred to a nursing unit that's appropriate for the patient's condition and postoperative assessment needs. An ambulatory surgical patient (outpatient) can usually go home with detailed instructions and referral to the surgeon for follow-up care.
Clinical alert: Drainage on the dressing should be minimal. If it's excessive or if the site appears abnormal, report your finding to the surgeon.If you're discharging the patient with tubes, catheters, drains, or IV catheters, verify that they're patent and secured properly.
Screen for and assess the patient’s pain using facility-defined criteria that are consistent with the patient’s age, condition, and ability to understand.
Treat the patient’s pain, as needed and ordered, using nonpharmacologic, pharmacologic, or a combination of approaches. Base the treatment plan on evidence-based practices and the patient’s clinical condition, past medical history, and pain management goals.
Assess the patient's level of nausea and note any vomiting. Intervene and administer medications, as needed and ordered, following safe medication administration practices to treat the patient's nausea and vomiting.
Evaluate the patient's emotional status and provide comfort and support, as needed. Surgery is a life-changing experience. The patient may have difficulty dealing with the diagnosis or the outcomes of surgery.
Use a facility-approved post anesthesia scoring system, such as the Modified Aldrete Score, as indicated, to assess the patient's readiness for discharge from the PACU. If a scoring system isn't used in your facility, determine the patient's readiness for discharge according to your facility's discharge criteria as directed.
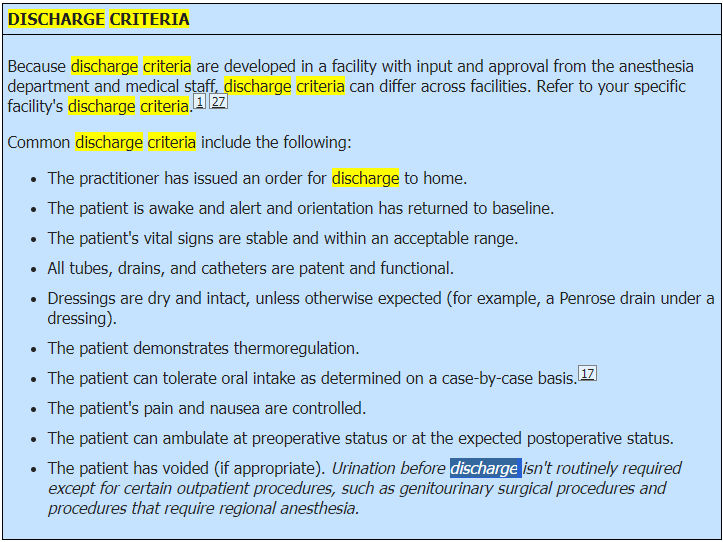
Prepare for discharge when the patient meets the discharge criteria. (See Discharge criteria.)
If discharging the patient to home, review the discharge instructions and provide a written copy of those instructions. Include the family or caregiver, as appropriate. Instructions should be written in the patient's and caregiver's native language. If instructions aren't available in the patient's native language, contact a medical interpreter. Provide the patient and caregiver with contact information for additional resources, including phone numbers for the health care facility, surgeon, emergency services, and home care or support groups, as applicable, in case problems arise.
As indicated, request return demonstrations from the patient and family for necessary post discharge procedures, such as medication administration, care of dressings and drains, and proper use of equipment, to evaluate their understanding of post discharge needs.
Review follow-up appointments and care with the patient. Provide this information in written form.
If discharging to home, assist the patient with dressing, as needed.
If transferring the patient to an inpatient unit, provide handoff communication for the person who will assume responsibility for the patient's care. Allow time for questions, as needed, to avoid miscommunications that may cause patient care errors during transitions of care. As part of the handoff process, allow time for the receiving staff member to trace each tubing and catheter from the patient to its point of origin; a standardized line reconciliation process should be used.
For a patient who will be discharged directly home, make sure that a responsible person is present to accompany the patient home. Ensure that the patient has safe transportation; the patient may not drive home. If the patient lacks appropriate transportation, consult with care management (or follow the channels identified by your facility) and notify the patient's practitioner. If the patient requires evaluation and treatment during transport to a discharge location, make sure that a registered nurse assists with the transport